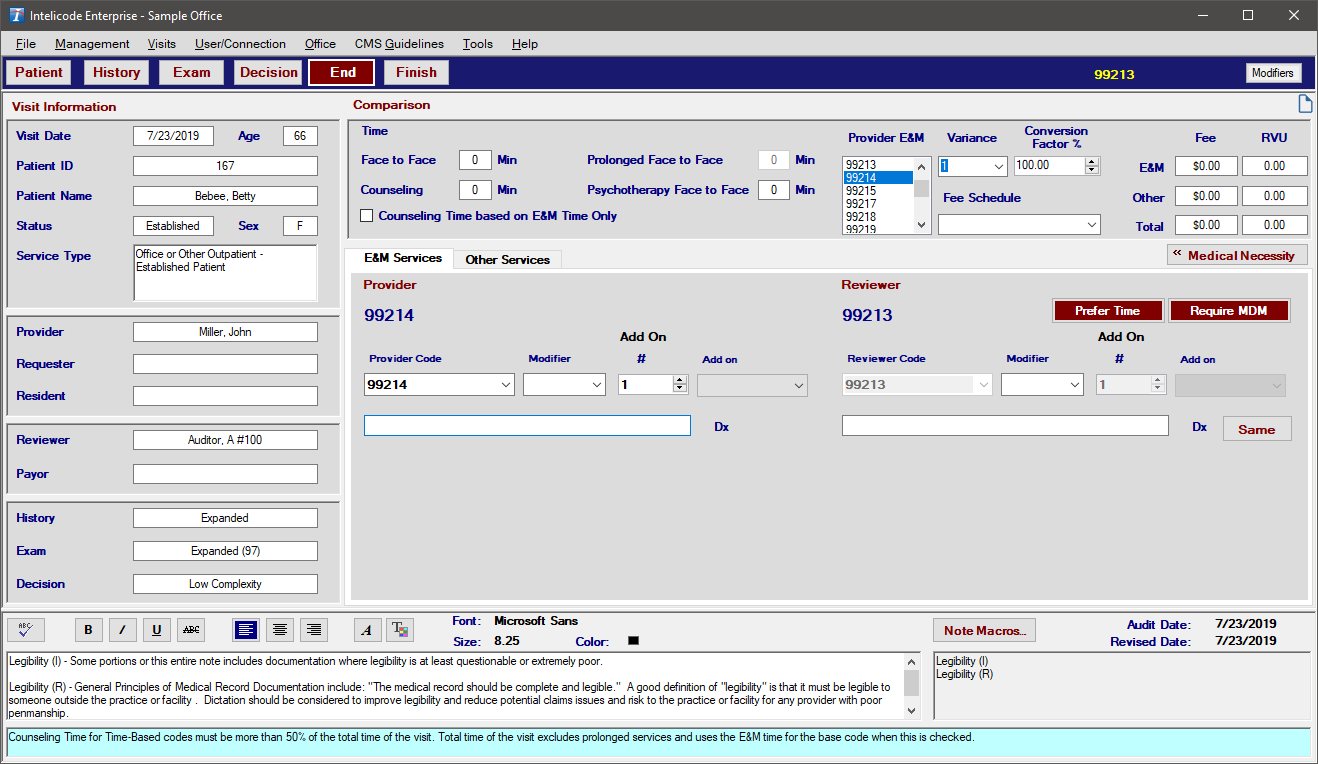
1.To indicate the Provider or Billed code, click on the appropriate (or not so appropriate as the case may be) code in the list of E&M codes under the Provider E&M heading on the End Screen, and Intelicode® will calculate a Variance and an Overbilled or Underbilled amount (based on your currently selected fee schedule).
2.If you don't have a fee schedule, you can still report on those services that are inappropriately coded. The Variance is calculated by looking at the Service Category.
3.For example, if the software calculates a 99213 and the provider billed a 99214, Intelicode® will see that both codes are from the same category (99211-99215) and calculates the difference between the Provider (Billed) and Reviewer (Audited) code.
4.Regardless of whether or not you use a Fee Schedule, Intelicode will keep a running total on Overbilled, Underbilled, Wrong Category, and Non-Compliant Teaching Physician visits.
Copyright © 1998-2026 Technology Solutions, Inc. All rights reserved.
INTELICODE® is a registered trademark of Technology Solutions, Inc. (TSI). All Rights Reserved.